Morton’s Neuroma Is a Nerve Condition
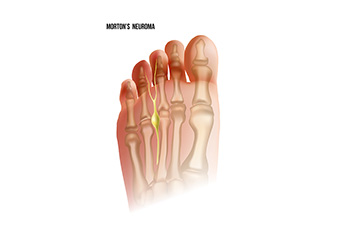
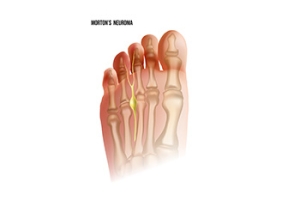
Morton's neuroma, a painful foot condition, stems from the compression of the plantar digital nerve, typically between the third and fourth toes. This nerve compression leads to the thickening of the nerve tissue, resulting in sharp, burning pain, tingling sensations, and numbness in the affected toes. Despite its name, Morton's neuroma is not a true neuroma, or tumor, but rather a nerve entrapment or irritation. The precise cause of Morton's neuroma remains unclear, though factors such as repetitive stress, wearing tight or high-heeled shoes, foot deformities, and certain activities that involve pressure on the forefoot are thought to contribute to its development. Diagnosis often involves a thorough examination by a podiatrist, including a physical assessment of the foot. This may include imaging tests like X-rays or MRI scans to confirm the condition. If you are experiencing pain in this part of your foot, it is suggested that you consult a podiatrist who can accurately diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Eveleigh Williams, DPM of Sole 2 Sole, PC. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Olympia Fields, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What is Morton's Neuroma?
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
Cracked Heels and Vitamin Deficiencies

Cracked heels can be attributed to various factors, including inadequate nutrition and vitamin deficiencies. Several vitamins play essential roles in maintaining healthy skin, and their deficiencies can contribute to dryness and cracking. For instance, vitamin E acts as an antioxidant, protecting skin cells from damage and promoting moisture retention. Vitamin C is vital for collagen synthesis, which helps maintain skin elasticity and integrity. Similarly, vitamin A supports skin cell turnover and repair, preventing dryness and fissures. Deficiencies in these vitamins, often stemming from poor dietary intake or underlying health conditions, can weaken the skin's barrier function and make it more susceptible to cracking in areas of high pressure like the heels. To address cracked heels caused by vitamin deficiencies, incorporating nutrient-rich foods into the diet or taking supplements under medical supervision can help promote skin health and prevent further complications. Cracked heels can be uncomfortable, and if you have this condition, it is suggested that you are under the care of a podiatrist who can offer you prescribed medication and any other treatment necessary for relief.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Eveleigh Williams, DPM from Sole 2 Sole, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Olympia Fields, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
Treatment for Bunions Including Surgery

A bunion is a bony protrusion at the base of the big toe that can cause significant discomfort and affect daily activities. Luckily, there are various bunion treatment options available to alleviate symptoms and restore foot function. For mild to moderate cases, nonsurgical approaches include wearing wider shoes with supportive soles, using bunion shields and pads, and taking anti-inflammatory medications. Night splints and toe separators may also help correct toe alignment and stretch tight soft tissues. Custom orthotics can address foot mechanics and prevent further progression of the deformity. When conservative measures fail to bring relief, surgical intervention may be necessary. Bunion surgery, or bunionectomy, aims to correct the misalignment of the big toe joint and remove bony growths. This type of surgery is not without risks and may not always be successful. Therefore, early recognition, accurate diagnosis, and appropriate treatment are a must. A podiatrist can help to develop a personalized treatment plan that is best tailored to your needs. If you are struggling with persistent bunion pain, it is suggested that you schedule an appointment with a podiatrist.
If you are suffering from bunions, contact Eveleigh Williams, DPM of Sole 2 Sole, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Olympia Fields, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
When Do I Need to See a Podiatrist?

Foot problems can signal underlying health issues that can worsen if ignored. For instance, neuropathy, resulting from nerve damage, can lead to numbness in the feet and make it hard to detect injuries. Conditions like diabetes frequently result in neuropathy, but a podiatrist is medically trained to offer treatments to manage symptoms. Changes in foot color can signal underlying issues like infections or poor circulation, and identifying and addressing these issues early is essential for effective treatment. Bunions, a deformity of the big toe, can cause discomfort and reduce mobility, but a podiatrist can recommend suitable footwear and a variety of treatment options to alleviate discomfort. Whether from high-impact exercises or wearing improper footwear, foot soreness should not be ignored. Podiatrists can prescribe custom orthotics to help alleviate pain and improve gait problems. Various musculoskeletal disorders can cause foot pain, and podiatrists can provide medication, foot padding, and other treatments to manage symptoms and improve mobility. If you have foot problems that interfere with daily activities, it is suggested that you schedule an appointment with a podiatrist.
If you are dealing with pain in your feet and ankles, you may want to seek help from a podiatrist. Feel free to contact Eveleigh Williams, DPM from Sole 2 Sole, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
A podiatrist is a doctor of podiatric medicine who diagnoses and treats conditions of the foot, ankle, and related structures of the leg. Your podiatrist may specialize in a certain field such as sports medicine, wound care, pediatrics, and diabetic care. Podiatrists have the ability to become board certified through training, clinical experience, and then taking an exam.
What Do Podiatrists Do?
On a daily basis, a podiatrist may perform the following activities:
- Diagnose foot ailments such as ulcers, tumors, fractures, etc.
- Use innovative methods to treat conditions
- Use corrective orthotics, casts, and strappings to correct deformities
- Correct walking patterns and balance
- Provide individual consultations to patients
It is very important that you take care of your feet. It’s easy to take having healthy feet for granted, however foot problems tend to be among the most common health conditions. Podiatrists can help diagnose and treat a variety of feet related conditions, so it is crucial that you visit one if you need assistance.
If you have any questions please feel free to contact our office located in Olympia Fields, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
The branch of medicine that is focused on the treatment, diagnosis, and study of disorders of the lower leg, ankle and foot is referred to as podiatry. Because people often spend a great deal of their time on their feet, many problems in this area can occur. A person seeks help from the field of podiatry when they need treatment for heel spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, infections, and problems with the foot that are related to diabetes and additional diseases.
To treat problems of the foot, ankle or lower leg, a podiatrist may prescribe physical therapy, drugs, perform surgery, or set fractures. Individuals may also be recommended to wear corrective shoe inserts, custom-made shoes, plaster casts and strappings in order to correct deformities.
When trying to gather information on a patient problem, a scanner or force plate may be used in order to design orthotics. During this procedure, patients are told to walk across a plate that is connected to a computer; the computer then takes a scan of the foot and indicates weight distribution and pressure points. The computer readouts will give the podiatrist information to help them determine the correct treatment plans.
Diagnosis is also provided through laboratory tests and x-rays. Through the foot, the first signs of serious problems such as heart disease, diabetes and arthritis can show up. For example, individuals that have diabetes may frequently have problems such as infections and foot ulcers because they experience poor circulation in the foot area. A podiatrist can then have consultations with patients when symptoms arise. Referrals will then be made to specialists that handle the greater health problems.
Some podiatrists have their own independent, private practices or clinics where they have a small staff and administrative personnel. Many podiatrists work within group practices. They usually spend time performing surgery in ambulatory surgical centers or hospitals, or visit patients in nursing homes. Podiatrists typically spend between 30 to 60 hours of week working. Some podiatrists specialize in public health, orthopedics, surgery, or primary care. Other fields include specialties in geriatrics, dermatology, pediatrics, diabetic foot care and sports medicine.
Some podiatrist specialists complete extra training in the area of foot and ankle reconstruction that results from the effects of physical trauma or diabetes. There are also surgeons that perform surgery of a cosmetic nature to correct bunions and hammertoes.
Plantar Heel Pain
 Plantar heel pain, often referred to as plantar fasciitis, can cause discomfort and interfere with daily activities. It typically occurs when the band of tissue that supports the arch of the foot, called the plantar fascia, becomes irritated or inflamed. This condition often brings sharp pain in the heel, especially when taking the first steps in the morning or after prolonged periods of rest. Plantar heel pain can be triggered by various factors, including overuse, improper footwear, obesity, or certain foot structures. A podiatrist, or foot doctor, may recommend treatments such as stretching exercises, orthotic inserts, or in severe cases, corticosteroid injections and possibly surgery. With proper care and treatment, most people can find relief from plantar heel pain and get back to enjoying their daily activities without discomfort. If you are suffering from heel pain, it is suggested that you make an appointment with a podiatrist.
Plantar heel pain, often referred to as plantar fasciitis, can cause discomfort and interfere with daily activities. It typically occurs when the band of tissue that supports the arch of the foot, called the plantar fascia, becomes irritated or inflamed. This condition often brings sharp pain in the heel, especially when taking the first steps in the morning or after prolonged periods of rest. Plantar heel pain can be triggered by various factors, including overuse, improper footwear, obesity, or certain foot structures. A podiatrist, or foot doctor, may recommend treatments such as stretching exercises, orthotic inserts, or in severe cases, corticosteroid injections and possibly surgery. With proper care and treatment, most people can find relief from plantar heel pain and get back to enjoying their daily activities without discomfort. If you are suffering from heel pain, it is suggested that you make an appointment with a podiatrist.
Many people suffer from bouts of heel pain. For more information, contact Eveleigh Williams, DPM of Sole 2 Sole, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Olympia Fields, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.